Radiology Tech and Support: How We Keep You Reading
Many radiologists know vRad as a teleradiology practice, but what many may not realize is that it’s also a tech company. In fact, more than a third...

Remote radiologist jobs with flexible schedules, equitable pay, and the most advanced reading platform. Discover teleradiology at vRad.

Radiologist well-being matters. Explore how vRad takes action to prevent burnout with expert-led, confidential support through our partnership with VITAL WorkLife. Helping radiologists thrive.

Visit the vRad Blog for radiologist experiences at vRad, career resources, and more.

vRad provides radiology residents and fellows free radiology education resources for ABR boards, noon lectures, and CME.

Teleradiology services leader since 2001. See how vRad AI is helping deliver faster, higher-quality care for 50,000+ critical patients each year.

Subspecialist care for the women in your community. 48-hour screenings. 1-hour diagnostics. Comprehensive compliance and inspection support.

vRad’s stroke protocol auto-assigns stroke cases to the top of all available radiologists’ worklists, with requirements to be read next.

vRad’s unique teleradiology workflow for trauma studies delivers consistently fast turnaround times—even during periods of high volume.

vRad’s Operations Center is the central hub that ensures imaging studies and communications are handled efficiently and swiftly.

vRad is delivering faster radiology turnaround times for 40,000+ critical patients annually, using four unique strategies, including AI.
.jpg?width=1024&height=576&name=vRad-High-Quality-Patient-Care-1024x576%20(1).jpg)
vRad is developing and using AI to improve radiology quality assurance and reduce medical malpractice risk.

Now you can power your practice with the same fully integrated technology and support ecosystem we use. The vRad Platform.

Since developing and launching our first model in 2015, vRad has been at the forefront of AI in radiology.

Since 2010, vRad Radiology Education has provided high-quality radiology CME. Open to all radiologists, these 15-minute online modules are a convenient way to stay up to date on practical radiology topics.

Join vRad’s annual spring CME conference featuring top speakers and practical radiology topics.

vRad provides radiology residents and fellows free radiology education resources for ABR boards, noon lectures, and CME.

Academically oriented radiologists love practicing at vRad too. Check out the research published by vRad radiologists and team members.

Learn how vRad revolutionized radiology and has been at the forefront of innovation since 2001.

%20(2).jpg?width=1008&height=755&name=Copy%20of%20Mega%20Nav%20Images%202025%20(1008%20x%20755%20px)%20(2).jpg)

Visit the vRad blog for radiologist experiences at vRad, career resources, and more.


Explore our practice’s reading platform, breast imaging program, AI, and more. Plus, hear from vRad radiologists about what it’s like to practice at vRad.

Ready to be part of something meaningful? Explore team member careers at vRad.
3 min read
 Imad B. Nijim
:
April 3, 2019
Imad B. Nijim
:
April 3, 2019

Moving past the initial media hype, practitioners are beginning to demonstrate how AI applications can enhance the ability of radiologists to support better patient outcomes.
It’s a fact of life in our digital age that emerging technologies are often accompanied by overinflated expectations about their potential to transform the world.
Consider drones. Early supporters predicted that drones would soon shower our neighborhoods with smiling Amazon boxes and hover at our doors with hot Domino’s pizzas. Of course, they’ve since recognized many barriers to the drone distribution model. Setting aside original forecasts, engineers are finding many uses for drone technology in everyday applications.
With the exciting prospect of artificial intelligence in diagnostic imaging, prognosticators foretold of an overnight medical revolution – some even predicted that computers would eventually replace the need for physicians altogether. Thankfully, we are moving beyond the initial hype. For example, healthcare leaders are asking practical questions to leverage AI to improve patient care through better workflow, higher quality reporting and optimized efficiency. As a result, we seamlessly weave practical AI algorithms into daily workflows with the goal of enabling physicians to deliver the best care possible.
Diagnostic imaging is an area of great potential for practical AI.
Image-based and natural language processing (NLP) models are being implemented today into clinical workflows and have demonstrated early success. For example, smart worklists are using AI to prioritize studies to ensure the right study is presented to the right radiologist. Other AI models are built to relieve radiologists of relatively mundane tasks, so they can focus on delivering high quality interpretations. In short, AI enables radiologists to focus their expertise where it matters most.
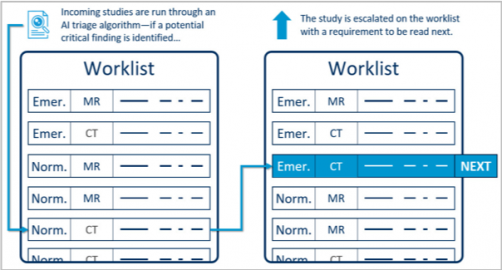
As an example, AI is proving to be a valuable triage tool. In an optimized radiology environment, studies that are part of a trauma or stroke protocol are prioritized in the physician’s worklist. Studies that are not part of a trauma or stroke protocol, sometimes contain a condition that requires expedited attention. A facility may request an interpretation of images “non-emergently,” but the patient may be experiencing an urgent condition – such as intra-cranial hemorrhage, pulmonary embolism or aortic dissection. AI can look at the images and identify the study for proper prioritization in the worklist.
It is important to note that each model’s individual performance, as measured by sensitivity and specificity, will determine the viability of its use in a production environment. Each model must be refined to meet acceptable thresholds for false positives and false negatives before it can be employed effectively in any workflow.
We’ve just begun to scratch the surface of all that is possible. A single triage workflow may employ tens or even hundreds of models. However, there are less complex models showing great promise for driving operational improvements. For example, one AI model in use determines how many images are in a chest x-ray, even when there are multiple images on the same pixel matrix. Another model determines if the chest x-ray is lateral or frontal (AP/PA). Both of these relatively simple models have immediate practical benefits as a surprisingly large percentage of chest x-ray studies are ordered with incomplete or inaccurate metadata. This quick fix of the metadata using AI avoids potential billing errors and will ensure the images are displayed properly without interrupting the radiologist.
As AI proves its value to radiologists, radiologists are embracing and facilitating the evolution of AI.
The future of radiology is rooted in a collaborative partnership between imaging practitioners and systems engineers. Ultimately, the goal is to improve overall quality, which also improves efficiency. Success requires AI integration into the practical workflow. Automating mundane tasks that are better handled by a computer should eliminate distractions and reduce error rates. Meanwhile, each diagnostic report, through the use of NLP provides essential data to fuel the continued improvement in AI for radiology.
Achieving the full potential of practical AI in radiology requires a strong analytics foundation and deep workflow integration. It requires continuous collaboration between technical leadership and clinical leadership. On a daily basis, they must evaluate AI use cases and ask one another: What problems can we solve? What task can be automated? What are the results? How might we improve patient care?
It is exciting to work in a field that embraces new technologies and AI is poised to be transformational on multiple levels. As we build and deploy AI models, early successes are generating excitement and hope for continued innovation that will enable radiologists to enhance standards of care.
Reposted from Healthcare Business News.
Back to Blog
.png)
Many radiologists know vRad as a teleradiology practice, but what many may not realize is that it’s also a tech company. In fact, more than a third...

Welcome back to the vRad technology quest as we unlock the 7th and final key! As always, I recommend you check out the first post in the series if...
.png)
For the latest information on vRad’s Artificial Intelligence program please visit vrad.com/radiology-services/radiology-ai/ ...
vRad (Virtual Radiologic) is a national radiology practice combining clinical excellence with cutting-edge technology development. Each year, we bring exceptional radiology care to millions of patients and empower healthcare providers with technology-driven solutions.
Non-Clinical Inquiries (Total Free):
800.737.0610
Outside U.S.:
011.1.952.595.1111
3600 Minnesota Drive, Suite 800
Edina, MN 55435