12 Radiologist Safety Nets to Reduce Stress, Improve Care, and Make Radiology Enjoyable Again
This is the first in a series of blog posts we’re calling “@vRad” where radiologists can get a sneak peek behind the curtain to see what it’s like to...

Remote radiologist jobs with flexible schedules, equitable pay, and the most advanced reading platform. Discover teleradiology at vRad.

Radiologist well-being matters. Explore how vRad takes action to prevent burnout with expert-led, confidential support through our partnership with VITAL WorkLife. Helping radiologists thrive.

Visit the vRad Blog for radiologist experiences at vRad, career resources, and more.

vRad provides radiology residents and fellows free radiology education resources for ABR boards, noon lectures, and CME.

Teleradiology services leader since 2001. See how vRad AI is helping deliver faster, higher-quality care for 50,000+ critical patients each year.

Subspecialist care for the women in your community. 48-hour screenings. 1-hour diagnostics. Comprehensive compliance and inspection support.

vRad’s stroke protocol auto-assigns stroke cases to the top of all available radiologists’ worklists, with requirements to be read next.

vRad’s unique teleradiology workflow for trauma studies delivers consistently fast turnaround times—even during periods of high volume.

vRad’s Operations Center is the central hub that ensures imaging studies and communications are handled efficiently and swiftly.

vRad is delivering faster radiology turnaround times for 40,000+ critical patients annually, using four unique strategies, including AI.
.jpg?width=1024&height=576&name=vRad-High-Quality-Patient-Care-1024x576%20(1).jpg)
vRad is developing and using AI to improve radiology quality assurance and reduce medical malpractice risk.

Now you can power your practice with the same fully integrated technology and support ecosystem we use. The vRad Platform.

Since developing and launching our first model in 2015, vRad has been at the forefront of AI in radiology.

Since 2010, vRad Radiology Education has provided high-quality radiology CME. Open to all radiologists, these 15-minute online modules are a convenient way to stay up to date on practical radiology topics.

Join vRad’s annual spring CME conference featuring top speakers and practical radiology topics.

vRad provides radiology residents and fellows free radiology education resources for ABR boards, noon lectures, and CME.

Academically oriented radiologists love practicing at vRad too. Check out the research published by vRad radiologists and team members.

Learn how vRad revolutionized radiology and has been at the forefront of innovation since 2001.

%20(2).jpg?width=1008&height=755&name=Copy%20of%20Mega%20Nav%20Images%202025%20(1008%20x%20755%20px)%20(2).jpg)

Visit the vRad blog for radiologist experiences at vRad, career resources, and more.


Explore our practice’s reading platform, breast imaging program, AI, and more. Plus, hear from vRad radiologists about what it’s like to practice at vRad.

Ready to be part of something meaningful? Explore team member careers at vRad.
2 min read
 Juan Batlle, MD
:
April 25, 2018
Juan Batlle, MD
:
April 25, 2018

Today we have the capability—unparalleled in human history—to compile enormous amounts of information, then apply sophisticated analytic tools and artificial intelligence to help solve patients’ most vexing difficulties. Managing big data is essential to building specialized centers of excellence, and diagnostic imaging is a vital part of their success.
Precision medicine is the natural evolution of medical practice. We’ve been attempting to achieve precision medicine for thousands of years. The ancient world labeled patients with "fever"; by the 19th century we could inform this with the germ theory of disease; now we can isolate the subspecies of bacteria and measure susceptibility to antibiotics. We are starting to understand genes that can tell us what the effectiveness of those antibiotics will be, how long to take them, and who will develop side effects.
Today, technology is hyper-accelerating advancements in medical diagnoses and treatments. With it, we can compile huge volumes of data on virtually every pathology and condition, measured and observed through every branch of medicine, from the time a patient first presents, through every step of treatment, and beyond.
The Miami Cancer Institute (MCI) is a magnet for applied data from local and regional cancer experts, including every medical discipline and every support service engaged in providing world-class cancer care to patients across the Southeastern U.S. as well as Latin America and the Caribbean. I’m proud to be one of over 70 radiologists at Radiology Associates of South Florida (RASF) who are actively contributing findings and exploring opportunities for imaging to deliver more accurate cancer diagnoses, helping MCI clinicians provide the most appropriate care plan for each patient.
Of course, the goal of centers of excellence is not realized simply through data collection and analysis. The potential is released through communication, both within the defined center of excellence, and ultimately with the entire global medical community. This seems a good time for me to suggest you join the discussion May 1, at a webinar roundtable featuring five colleagues and myself from RASF: Building a Cancer Care Center of Excellence in the Age of Precision Medicine.
View the Webinar Recording
Every day I’m amazed by strides taken in the field of medicine. At the same time, the results of every study seem to raise new questions and new opportunities for discovery as we continue to hone the practice of precision medicine.
For example, The New England Journal of Medicine in April 2018 published a lung cancer study that demonstrated significantly longer and progression-free survival rates among patients who received immunotherapy and chemotherapy combined, versus those who received chemo alone. It’s an important study that certainly has the potential to elevate the standard of cancer care.
However, this study also reveals that, while the combination therapy increased overall survival rates, only half of those receiving the therapy actually responded to it, while the other half experienced little or no benefit. As a radiologist—and knowing the outcomes for each—I would be compelled to reexamine the imaging history of these patients. Perhaps we might unveil indicators—e.g. tumor shape, volume, growth rate, composition, location—that reveal early in the process which patients will respond well to this therapy, and which patients might best be treated through alternative methods.
Of course, it would be no small task for one rad to eyeball the complete diagnostic histories of the over 600 participants in this study—not to mention hundreds of new lung cancer cases diagnosed every day—to detect patterns or anomalies that correlate to patient outcomes.
Computers, on the other hand, are being be trained to do this quickly and efficiently, providing radiologists opportunities to see the big picture more clearly than ever before. Radiomics and artificial intelligence (AI) are two ways radiology will be able to continue to tailor diagnosis and therapy. Perhaps an AI engine will identify the patients who will benefit most from imaging and provide aids to diagnosis; radiomics of a lung nodule might give insight into which patients are most likely to harbor a cancer, or which cancer patients are most likely to benefit from a certain chemotherapy regimen.
Radiologists’ insights are essential to guiding centers of excellence to achieve their promise of personalized patient care.
Back to Blog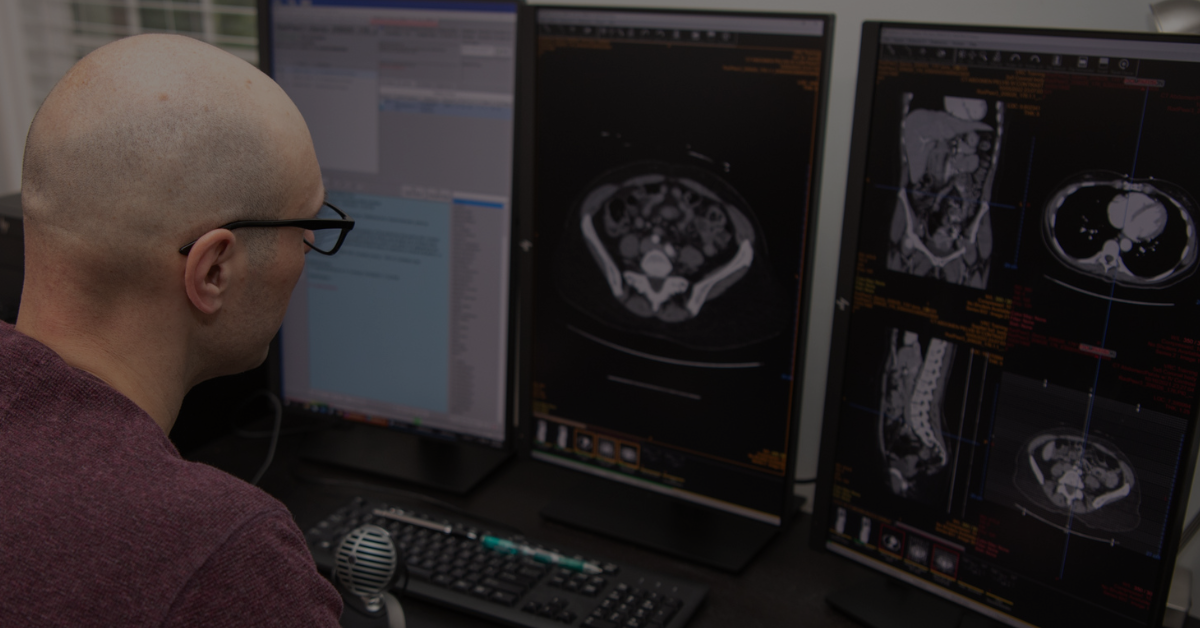
This is the first in a series of blog posts we’re calling “@vRad” where radiologists can get a sneak peek behind the curtain to see what it’s like to...

Through CGI (computer-generated imagery), the folks at Pixar – creators of Finding Nemo, Toy Story, and Monsters, Inc. – allow audiences to explore...

At vRad, we have a passion for connecting – with each other, with clients, and with patients. In technology, we strive to break down the language...
vRad (Virtual Radiologic) is a national radiology practice combining clinical excellence with cutting-edge technology development. Each year, we bring exceptional radiology care to millions of patients and empower healthcare providers with technology-driven solutions.
Non-Clinical Inquiries (Total Free):
800.737.0610
Outside U.S.:
011.1.952.595.1111
3600 Minnesota Drive, Suite 800
Edina, MN 55435