1 min read
Teleradiology Consults: Instant Assistance Anytime You Need It
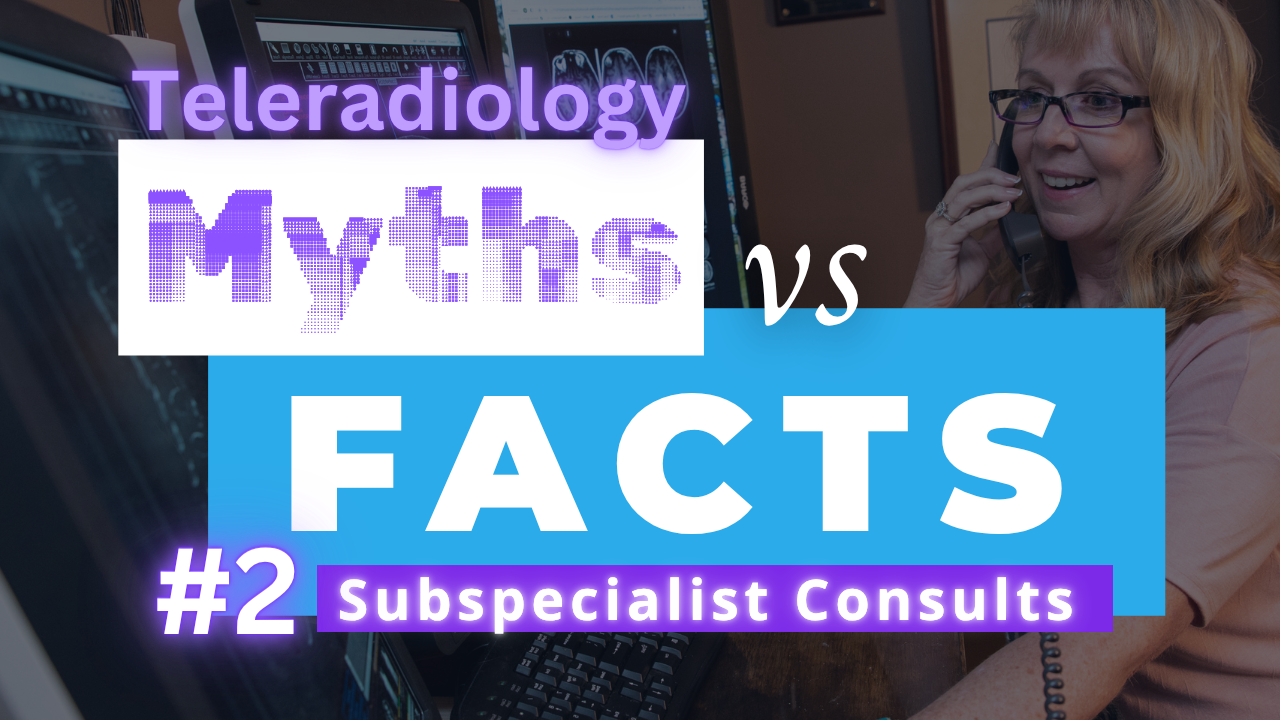
A common myth about teleradiology is that radiologists are siloed, without peer support. I found the exact opposite to be true.
Read More
Remote radiologist jobs with flexible schedules, equitable pay, and the most advanced reading platform. Discover teleradiology at vRad.

Radiologist well-being matters. Explore how vRad takes action to prevent burnout with expert-led, confidential support through our partnership with VITAL WorkLife. Helping radiologists thrive.

Visit the vRad Blog for radiologist experiences at vRad, career resources, and more.

vRad provides radiology residents and fellows free radiology education resources for ABR boards, noon lectures, and CME.

Teleradiology services leader since 2001. See how vRad AI is helping deliver faster, higher-quality care for 50,000+ critical patients each year.

Subspecialist care for the women in your community. 48-hour screenings. 1-hour diagnostics. Comprehensive compliance and inspection support.

vRad’s stroke protocol auto-assigns stroke cases to the top of all available radiologists’ worklists, with requirements to be read next.

vRad’s unique teleradiology workflow for trauma studies delivers consistently fast turnaround times—even during periods of high volume.

vRad’s Operations Center is the central hub that ensures imaging studies and communications are handled efficiently and swiftly.

vRad is delivering faster radiology turnaround times for 40,000+ critical patients annually, using four unique strategies, including AI.
.jpg?width=1024&height=576&name=vRad-High-Quality-Patient-Care-1024x576%20(1).jpg)
vRad is developing and using AI to improve radiology quality assurance and reduce medical malpractice risk.

Now you can power your practice with the same fully integrated technology and support ecosystem we use. The vRad Platform.

Since developing and launching our first model in 2015, vRad has been at the forefront of AI in radiology.

Since 2010, vRad Radiology Education has provided high-quality radiology CME. Open to all radiologists, these 15-minute online modules are a convenient way to stay up to date on practical radiology topics.

Join vRad’s annual spring CME conference featuring top speakers and practical radiology topics.

vRad provides radiology residents and fellows free radiology education resources for ABR boards, noon lectures, and CME.

Academically oriented radiologists love practicing at vRad too. Check out the research published by vRad radiologists and team members.

Learn how vRad revolutionized radiology and has been at the forefront of innovation since 2001.

%20(2).jpg?width=1008&height=755&name=Copy%20of%20Mega%20Nav%20Images%202025%20(1008%20x%20755%20px)%20(2).jpg)

Visit the vRad blog for radiologist experiences at vRad, career resources, and more.


Explore our practice’s reading platform, breast imaging program, AI, and more. Plus, hear from vRad radiologists about what it’s like to practice at vRad.

Ready to be part of something meaningful? Explore team member careers at vRad.

Remote radiologist jobs with flexible schedules, equitable pay, and the most advanced reading platform. Discover teleradiology at vRad.

Radiologist well-being matters. Explore how vRad takes action to prevent burnout with expert-led, confidential support through our partnership with VITAL WorkLife. Helping radiologists thrive.

Visit the vRad Blog for radiologist experiences at vRad, career resources, and more.

vRad provides radiology residents and fellows free radiology education resources for ABR boards, noon lectures, and CME.

Teleradiology services leader since 2001. See how vRad AI is helping deliver faster, higher-quality care for 50,000+ critical patients each year.

Subspecialist care for the women in your community. 48-hour screenings. 1-hour diagnostics. Comprehensive compliance and inspection support.

vRad’s stroke protocol auto-assigns stroke cases to the top of all available radiologists’ worklists, with requirements to be read next.

vRad’s unique teleradiology workflow for trauma studies delivers consistently fast turnaround times—even during periods of high volume.

vRad’s Operations Center is the central hub that ensures imaging studies and communications are handled efficiently and swiftly.

vRad is delivering faster radiology turnaround times for 40,000+ critical patients annually, using four unique strategies, including AI.
.jpg?width=1024&height=576&name=vRad-High-Quality-Patient-Care-1024x576%20(1).jpg)
vRad is developing and using AI to improve radiology quality assurance and reduce medical malpractice risk.

Now you can power your practice with the same fully integrated technology and support ecosystem we use. The vRad Platform.

Since developing and launching our first model in 2015, vRad has been at the forefront of AI in radiology.

Since 2010, vRad Radiology Education has provided high-quality radiology CME. Open to all radiologists, these 15-minute online modules are a convenient way to stay up to date on practical radiology topics.

Join vRad’s annual spring CME conference featuring top speakers and practical radiology topics.

vRad provides radiology residents and fellows free radiology education resources for ABR boards, noon lectures, and CME.

Academically oriented radiologists love practicing at vRad too. Check out the research published by vRad radiologists and team members.

Learn how vRad revolutionized radiology and has been at the forefront of innovation since 2001.

%20(2).jpg?width=1008&height=755&name=Copy%20of%20Mega%20Nav%20Images%202025%20(1008%20x%20755%20px)%20(2).jpg)

Visit the vRad blog for radiologist experiences at vRad, career resources, and more.


Explore our practice’s reading platform, breast imaging program, AI, and more. Plus, hear from vRad radiologists about what it’s like to practice at vRad.

Ready to be part of something meaningful? Explore team member careers at vRad.
1 min read
A common myth about teleradiology is that radiologists are siloed, without peer support. I found the exact opposite to be true.
Read More
1 min read
AJR podcast with guest Dr. Ben Strong, vRad CMO

3 min read
“I couldn’t believe it was so easy.” It’s one of the most common things I hear from radiologists who’ve recently joined vRad when I meet with them in...
2 min read
It wasn’t one thing; it was everything. Interruptions, admin overload, staying late—radiology became overwhelming. I was burned out and fatigued and...

3 min read
A Community at Risk As the Director of Radiology at Hocking Valley Community Hospital, I have seen firsthand the challenges of providing specialized...
6 min read
Let’s start with the straight answer you’re looking for: At vRad, we have radiologists who make $450,000 a year, and high-volume readers who pull in...

2 min read
In celebration of World Radiology Day, we’re pleased to bring you an update on the incredible impact of the First Read Initiative (FRI) over the past...

5 min read
“Only a few more months and life will be good!” It’s the rallying cry of radiology residents and fellows everywhere. The idea that if we can just...

3 min read
Recently, 331 radiologists provided a glimpse into vRad by participating in Gallagher’s nationally benchmarked engagement survey of 12,000...
vRad (Virtual Radiologic) is a national radiology practice combining clinical excellence with cutting-edge technology development. Each year, we bring exceptional radiology care to millions of patients and empower healthcare providers with technology-driven solutions.
Non-Clinical Inquiries (Total Free):
800.737.0610
Outside U.S.:
011.1.952.595.1111
3600 Minnesota Drive, Suite 800
Edina, MN 55435